Understanding the triggers of COPD flare-ups is crucial for effective management and prevention.
Chronic Obstructive Pulmonary Disease (COPD) is a progressive lung disease that makes it difficult to breathe. For those living with this condition, flare-ups can be particularly distressing and often lead to hospital visits. Understanding what causes a COPD flare-up is essential for managing symptoms and maintaining a better quality of life.
The Nature of COPD and Its Flare-Ups
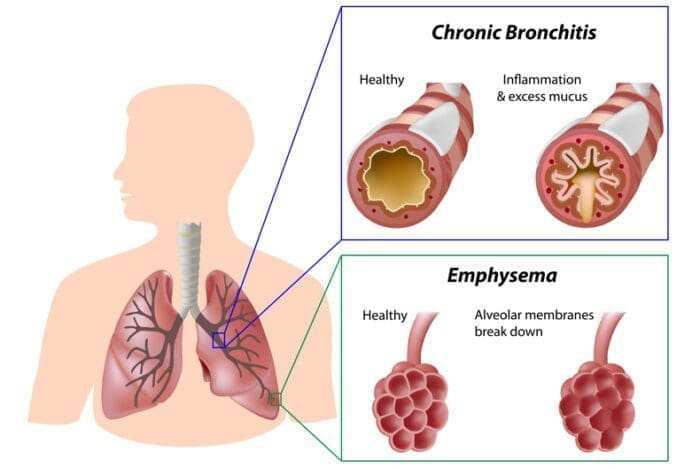
COPD encompasses several lung conditions, including emphysema and chronic bronchitis. These conditions cause airflow obstruction, leading to difficulty breathing, coughing, wheezing, and chest tightness. A flare-up occurs when these symptoms worsen significantly over a short period. This exacerbation can be triggered by various factors.
It’s important to recognize that flare-ups not only impact the individual’s health but can also lead to increased healthcare costs and reduced overall well-being. Managing these episodes effectively requires understanding their causes, which can often be complex.
Main Causes of COPD Flare-Ups
Several factors contribute to the onset of COPD flare-ups. Identifying these triggers is vital for prevention strategies.
1. Respiratory Infections
Respiratory infections are among the most common causes of COPD flare-ups. These infections can be viral or bacterial in nature. The common cold, influenza, and pneumonia are typical culprits that exacerbate COPD symptoms. When the lungs become infected, inflammation increases, leading to heightened breathlessness and coughing.
Preventing respiratory infections involves getting vaccinated against influenza and pneumonia, practicing good hygiene, and avoiding close contact with sick individuals.
2. Environmental Pollutants
Air quality plays a significant role in lung health. Pollutants such as smoke from cigarettes, vehicle emissions, industrial discharges, and even indoor pollutants like mold can trigger flare-ups. Exposure to these irritants leads to inflammation in the airways, making it harder for individuals with COPD to breathe.
Taking steps to minimize exposure—such as using air purifiers indoors or avoiding outdoor activities on days with poor air quality—can help mitigate these risks.
3. Weather Changes
Weather fluctuations can significantly affect those with COPD. Cold air can constrict the airways, while hot and humid weather may increase the risk of dehydration and respiratory distress. Sudden changes in temperature or humidity levels can provoke flare-ups.
It’s beneficial to monitor weather reports closely and plan outdoor activities accordingly. Wearing a scarf over the mouth during cold weather or staying hydrated during hot days may help ease symptoms.
4. Allergens
Allergens like pollen, dust mites, pet dander, and mold can trigger allergic reactions in many people. For those with COPD, exposure to allergens may lead to increased airway inflammation and subsequent flare-ups.
Keeping living spaces clean by regularly dusting and vacuuming can reduce allergen exposure. Additionally, using hypoallergenic bedding materials or air filters may help alleviate symptoms during allergy season.
Recognizing Symptoms of a Flare-Up
Being aware of early signs of a flare-up allows for prompt action that could prevent severe complications or hospitalizations.
Common Symptoms
- Increased shortness of breath
- Persistent cough
- Changes in sputum color or volume
- Chest tightness
- Fatigue
Recognizing these symptoms early is crucial for effective intervention strategies.
Preventative Measures for Managing Flare-Ups
Taking proactive steps can significantly reduce the frequency and severity of COPD flare-ups.
1. Medication Adherence
Adhering strictly to prescribed medication regimens is vital for managing COPD effectively. Medications may include bronchodilators that relax airway muscles or corticosteroids that reduce inflammation in the lungs.
Regular check-ins with healthcare providers ensure that treatment plans remain effective and adjusted as needed based on symptom changes or disease progression.
2. Lifestyle Modifications
Making lifestyle changes can have profound effects on managing COPD symptoms:
- Quitting Smoking: Smoking cessation is perhaps the most significant lifestyle change one can make for lung health.
- Regular Exercise: Engaging in physical activity helps improve lung function over time.
- Healthy Diet: A balanced diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats supports overall health.
These changes contribute not only to better lung function but also enhance overall well-being.
3. Regular Monitoring
Keeping track of daily symptoms allows individuals to identify patterns related to their condition better—this includes noting environmental factors or activities preceding a flare-up.
Using peak flow meters helps monitor lung function at home; this information is invaluable during consultations with healthcare providers.
| COPD Management Strategies | Description |
|---|---|
| Medication Adherence | Consistently taking prescribed medications as directed. |
| Lifestyle Modifications | Implementing healthy habits like quitting smoking and exercising regularly. |
| Regular Monitoring | Tracking symptoms daily for patterns related to flare-ups. |
| Avoiding Triggers | Identifying personal triggers such as allergens or pollutants. |
| Nutritional Support | A balanced diet rich in nutrients aids overall health. |
The Role of Healthcare Providers in Managing Flare-Ups
Healthcare professionals play an essential role in managing COPD effectively through education about potential triggers and treatment options available.
Regular appointments allow healthcare providers to assess lung function through tests like spirometry and adjust treatment plans accordingly based on symptom severity or changes noted by patients themselves.
Additionally, pulmonary rehabilitation programs offer structured support through exercise training tailored specifically for individuals with lung disease along with education about self-management techniques aimed at reducing exacerbations over time.
The Importance of Support Systems
Having a strong support network enhances coping mechanisms when dealing with chronic illnesses like COPD:
- Family Support: Family members understanding how best they can assist during difficult times fosters an environment conducive to healing.
- Peer Groups: Connecting with others facing similar challenges provides emotional support while sharing coping strategies learned through personal experiences.
Support systems create an atmosphere where individuals feel empowered rather than isolated—this sense of community proves invaluable throughout one’s journey managing chronic illness effectively.
Key Takeaways: COPD Flare-Ups
➤ Understanding Triggers: Recognizing what causes flare-ups is essential.
➤ Infection Prevention: Respiratory infections can significantly worsen symptoms.
➤ Minimize Pollutants: Avoiding environmental irritants helps protect lung health.
➤ Weather Awareness: Monitoring weather changes can prevent symptom exacerbation.
➤ Support Systems Matter: Strong networks enhance coping and management of COPD.
➤ Support Systems Matter: Strong networks enhance coping and management of COPD.
Frequently Asked Questions: What Causes a COPD Flare Up?
What are the primary causes of a COPD flare-up?
The primary causes of a COPD flare-up include respiratory infections, environmental pollutants, weather changes, and allergens. Respiratory infections, whether viral or bacterial, can lead to increased inflammation in the lungs, exacerbating symptoms. Environmental pollutants such as smoke and vehicle emissions can also trigger flare-ups by irritating the airways. Additionally, sudden weather changes can affect breathing, while allergens like pollen and dust mites can provoke allergic responses that worsen COPD symptoms.
How can I identify a COPD flare-up early?
Identifying a COPD flare-up early involves being aware of specific symptoms that may signal worsening conditions. Common early signs include increased shortness of breath, persistent coughing, changes in sputum color or volume, chest tightness, and fatigue. Monitoring these symptoms closely is crucial for timely intervention. Keeping a daily log of symptoms can help individuals recognize patterns and triggers that precede flare-ups, allowing for proactive management strategies to be implemented effectively.
What lifestyle changes can help prevent COPD flare-ups?
Lifestyle changes play a significant role in preventing COPD flare-ups. Quitting smoking is the most impactful change one can make to enhance lung health. Regular exercise improves lung function and overall stamina. A healthy diet rich in fruits, vegetables, whole grains, and lean proteins supports immune health and helps manage weight. Additionally, staying hydrated and avoiding known triggers like allergens or pollutants further contributes to reducing the frequency of exacerbations.
How important is medication adherence in managing COPD?
Medication adherence is vital for managing COPD effectively. Consistently taking prescribed medications such as bronchodilators and corticosteroids helps control inflammation and improves lung function. Regular follow-ups with healthcare providers ensure that treatment plans remain effective as symptoms change or progress over time. Missing doses or not following the regimen can lead to increased symptoms and higher risks of severe flare-ups, making adherence an essential component of successful COPD management.
What role do healthcare providers play in managing COPD flare-ups?
Healthcare providers play an essential role in managing COPD by offering education about potential triggers and treatment options available. They conduct regular assessments of lung function through tests like spirometry to monitor disease progression. Providers also help develop personalized management plans tailored to individual needs based on symptom severity. Additionally, they may recommend pulmonary rehabilitation programs that combine exercise training with education on self-management techniques aimed at reducing exacerbations over time.
Conclusion – What Causes a COPD Flare Up?
Understanding what causes a COPD flare-up involves recognizing various triggers ranging from respiratory infections to environmental factors like pollution or allergens—all contributing significantly towards worsening symptoms experienced by those living with this chronic condition daily!
Proactive management strategies focusing on medication adherence alongside lifestyle modifications help mitigate risks associated with exacerbations while fostering healthier living environments ultimately leading towards improved quality-of-life outcomes over time!