Lobotomies, once a common psychiatric procedure, are now largely obsolete due to ethical concerns and advancements in mental health treatment.
The Historical Context of Lobotomy
Lobotomy, a neurosurgical procedure that involves severing connections in the brain’s prefrontal cortex, emerged in the early 20th century as a treatment for various mental disorders. The procedure gained traction during the 1930s and 1940s, primarily due to the work of Dr. António Egas Moniz, who believed that disrupting these neural pathways could alleviate severe psychiatric conditions. His pioneering work earned him the Nobel Prize in Physiology or Medicine in 1949, solidifying lobotomy’s place in medical history.
Initially hailed as a breakthrough, lobotomy was often performed on patients diagnosed with conditions ranging from schizophrenia to severe depression. The procedure was seen as a last resort for individuals who had not responded to other treatments. However, the lack of rigorous scientific validation and ethical oversight soon raised significant concerns about its safety and efficacy.
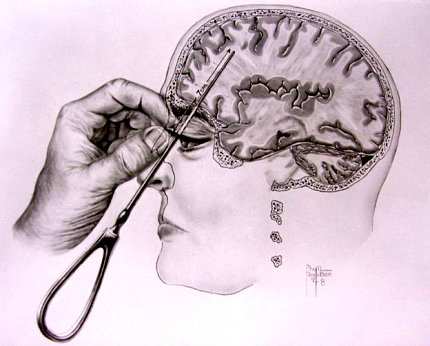
How Lobotomy Works
The lobotomy procedure typically involved drilling holes into the skull and inserting instruments to cut or destroy portions of the brain’s frontal lobes. There were various methods employed, including the transorbital lobotomy, which involved accessing the brain through the eye sockets using an instrument resembling an ice pick. This method became infamous for its quick execution and minimal surgical requirements.
Despite its initial popularity, many patients experienced severe side effects post-surgery. These included cognitive deficits, personality changes, emotional blunting, and even seizures. Reports of adverse outcomes began to surface in medical literature and public discourse, leading to growing scrutiny over the practice.
The Decline of Lobotomy
By the late 1950s and early 1960s, public opinion began to shift against lobotomy as awareness of its consequences grew. The advent of antipsychotic medications revolutionized mental health treatment during this period. Drugs like chlorpromazine offered effective alternatives without necessitating invasive procedures. As these medications became more widely available and accepted within psychiatric practice, they overshadowed lobotomy as a treatment option.
Furthermore, ethical considerations surrounding patient consent and autonomy came to the forefront. Many patients undergoing lobotomies were unable or unqualified to provide informed consent due to their mental health conditions. This realization sparked widespread condemnation from both medical professionals and human rights advocates.
The Ethical Dilemma
The ethical implications of performing lobotomies raised fundamental questions about patient rights and medical responsibility. As stories emerged detailing the devastating effects on patients’ lives—loss of personality, inability to function independently—society began to demand accountability from healthcare providers.
In response to mounting criticism and legal challenges, many hospitals ceased performing lobotomies altogether by the 1970s. The psychological community began reevaluating its approach to treating mental illness, focusing on compassionate care rather than punitive measures like surgical intervention.
Modern Alternatives to Lobotomy
Today’s mental health landscape is vastly different from that of past decades. With a greater understanding of psychiatric disorders and advancements in neuroscience, various non-invasive treatments have emerged as viable alternatives for managing mental health issues.
| Treatment Type | Description | Common Uses |
|---|---|---|
| Medication | Pharmaceutical drugs that target neurotransmitter imbalances. | Anxiety disorders, depression, schizophrenia. |
| Cognitive Behavioral Therapy (CBT) | A structured therapy focused on changing negative thought patterns. | Anxiety disorders, depression. |
| Electroconvulsive Therapy (ECT) | A procedure that induces controlled seizures through electrical stimulation. | Severe depression resistant to medication. |
| Transcranial Magnetic Stimulation (TMS) | A non-invasive technique using magnetic fields to stimulate nerve cells. | Major depressive disorder. |
| Mindfulness-Based Therapies | Treatments focusing on meditation and awareness techniques. | Anxiety disorders, stress management. |
These modern approaches prioritize patient well-being while ensuring informed consent is obtained before any treatment begins.
The Role of Advocacy Groups
Advocacy groups play a crucial role in shaping public perception regarding mental health treatments. Organizations such as NAMI (National Alliance on Mental Illness) work tirelessly to educate both patients and families about available options while promoting policies that protect patient rights.
These groups have also been instrumental in lobbying against outdated practices like lobotomy. They emphasize recovery-oriented approaches that empower individuals rather than subjecting them to potentially harmful interventions.
The Impact of Media Representation
Media portrayals significantly influence societal attitudes toward mental health treatments. Films like “One Flew Over the Cuckoo’s Nest” have brought attention not only to the plight of individuals within psychiatric institutions but also highlighted controversial practices such as lobotomy.
Such representations spark conversations about ethics in medicine while fostering empathy towards those affected by mental illness. As narratives evolve within popular culture—shifting from stigmatization towards understanding—they contribute positively towards reducing discrimination against individuals seeking help for their conditions.
Current Research Trends in Neuroscience
Neuroscience continues making strides toward understanding complex brain functions related to mental illness better than ever before. Researchers are exploring innovative techniques such as neurofeedback training—a method allowing individuals control over their brain activity through real-time feedback.
New technologies like functional MRI scans enable scientists to observe brain activity patterns associated with specific disorders more accurately than previous methods allowed. This progress opens doors for tailored interventions based on individual neurobiological profiles rather than relying solely on generalized approaches prevalent during earlier eras when lobotomy was common practice.
The Future Landscape of Mental Health Treatment
As we move forward into an era defined by rapid technological advancements coupled with evolving societal norms surrounding healthcare access—it’s clear that comprehensive approaches will dominate future conversations about treating mental illness effectively without resorting back into archaic practices like lobotomy.
Interdisciplinary collaborations involving psychologists, psychiatrists neurologists will pave pathways towards holistic solutions addressing root causes rather than merely alleviating symptoms temporarily—a significant departure from historical models reliant upon invasive procedures devoid of empirical support!
Key Takeaways: Lobotomies
➤ Lobotomies are obsolete: Ethical concerns have led to their decline.
➤ Historical significance: Once a common treatment, now viewed critically.
➤ Advancements in treatment: Modern alternatives prioritize patient well-being.
➤ Ethical implications: Patient consent and autonomy are now paramount.
➤ Role of advocacy: Organizations help reshape perceptions of mental health.
➤ Role of advocacy: Organizations help reshape perceptions of mental health.
Frequently Asked Questions: Lobotomies
What are the historical reasons behind the use of lobotomies?
Lobotomies were introduced in the early 20th century as a radical treatment for severe mental disorders. The procedure gained popularity due to its perceived effectiveness in alleviating symptoms of conditions like schizophrenia and severe depression. Dr. António Egas Moniz, who pioneered the technique, believed that severing connections in the prefrontal cortex could help patients. Initially, it was seen as a breakthrough; however, ethical concerns and adverse outcomes soon overshadowed its benefits.
The rise of lobotomy coincided with a lack of effective treatments for mental illness, leading to its adoption as a last-resort option for patients unresponsive to other therapies.
Are lobotomies still performed today?
No, lobotomies are no longer performed in modern medical practice. The procedure has been deemed unethical and ineffective compared to contemporary mental health treatments. As awareness of the harmful side effects grew, including cognitive deficits and personality changes, public opinion shifted strongly against lobotomy.
With the introduction of antipsychotic medications and various therapeutic approaches, healthcare professionals now prioritize less invasive methods that respect patient autonomy and informed consent.
What alternatives exist to lobotomies in modern psychiatry?
Today, numerous alternatives to lobotomy are available for treating mental health disorders. These include medications, such as antidepressants and antipsychotics, which target neurotransmitter imbalances effectively. Cognitive Behavioral Therapy (CBT) is another popular approach that helps individuals change negative thought patterns.
Other non-invasive options like Transcranial Magnetic Stimulation (TMS) and Electroconvulsive Therapy (ECT) have also emerged as viable treatments for severe depression and other conditions, focusing on patient well-being without resorting to invasive procedures.
How did public perception of lobotomy change over time?
The public perception of lobotomy underwent significant transformation from its initial acceptance to widespread condemnation. In the 1940s and 1950s, it was viewed as a groundbreaking treatment; however, reports detailing devastating side effects began surfacing.
This shift was further fueled by advocacy groups highlighting patient rights and ethical considerations regarding consent. By the 1970s, many hospitals ceased performing lobotomies altogether due to these growing concerns about their safety and efficacy.
What role do advocacy groups play in mental health treatment discussions?
Advocacy groups play a vital role in shaping discussions around mental health treatments by raising awareness about patient rights and promoting evidence-based practices. Organizations like NAMI (National Alliance on Mental Illness) work tirelessly to educate the public on available treatment options while lobbying against outdated practices like lobotomy.
These groups emphasize recovery-oriented approaches that empower individuals rather than subjecting them to potentially harmful interventions. Their efforts contribute significantly to reducing stigma surrounding mental illness and advocating for compassionate care.
Conclusion – Are Lobotomies Still A Thing?
Lobotomies are no longer performed today due largely ethical considerations alongside advancements made within psychiatry over recent decades! While they once represented hope for some suffering individuals—widespread recognition regarding their harmful consequences has led us away from such practices entirely! The focus now lies firmly rooted within compassionate care utilizing evidence-based methodologies designed prioritize patient autonomy while ensuring optimal outcomes achievable through innovative alternatives available today!