Acute closed angle glaucoma is a serious eye condition that can lead to rapid vision loss if left untreated.
Acute closed angle glaucoma is one of the most critical forms of glaucoma, a group of eye diseases that damage the optic nerve and can result in irreversible vision loss. Understanding this condition is essential, especially since it can develop suddenly and without warning. In this article, I’ll delve into the complexities of acute closed angle glaucoma, including its causes, symptoms, risk factors, diagnosis, treatment options, and preventive measures.
What Causes Acute Closed Angle Glaucoma?
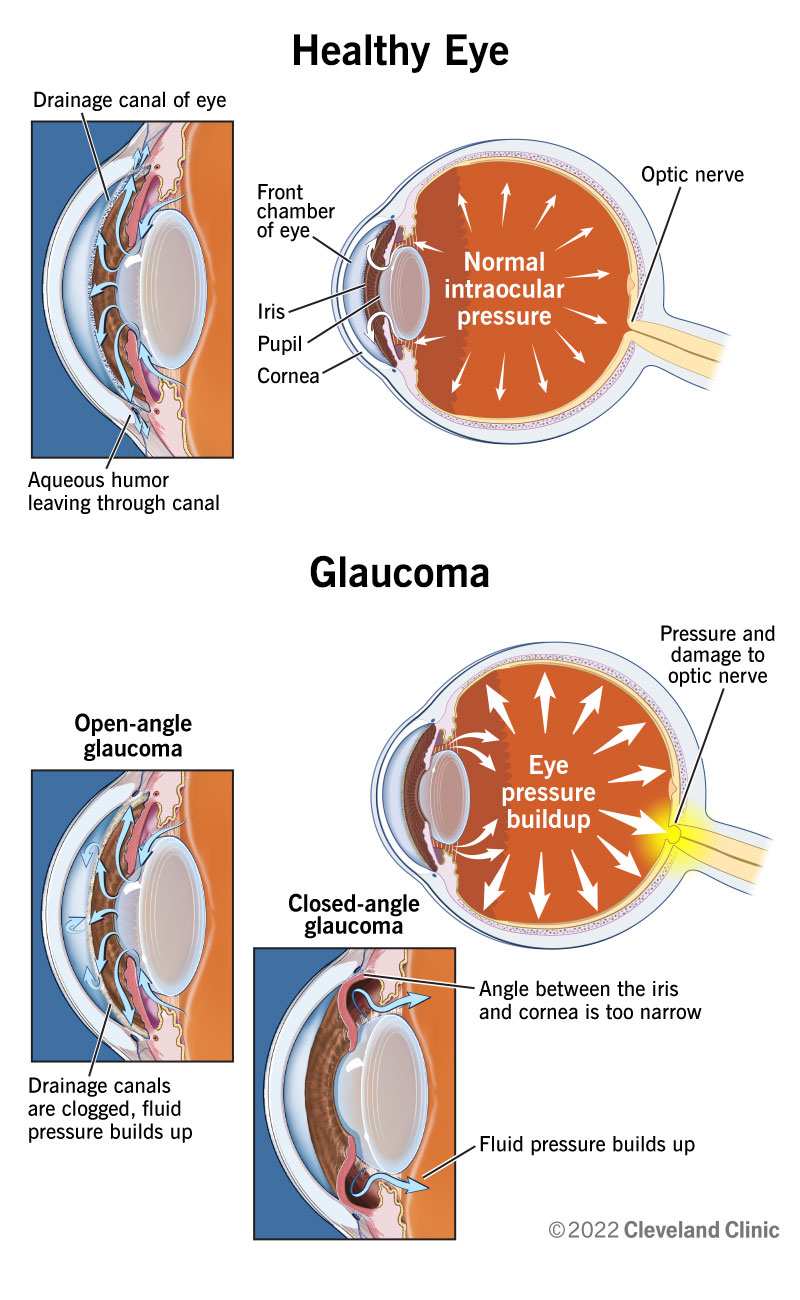
Acute closed angle glaucoma occurs when the drainage angle of the eye becomes blocked. This blockage prevents fluid from exiting the eye, leading to a rapid increase in intraocular pressure (IOP). The primary cause of this blockage is often anatomical. Some individuals have a naturally narrow angle between the iris and cornea, making them more susceptible to sudden episodes of increased pressure.
Other contributing factors can include certain medications that dilate the pupils, which can exacerbate the narrowing of the drainage angle. For instance, antihistamines and some antidepressants may trigger an acute attack in susceptible individuals. Moreover, age plays a significant role; as people age, changes in the structure of their eyes can increase their risk for developing this condition.
Recognizing Symptoms
Symptoms of acute closed angle glaucoma can appear suddenly and may include severe eye pain, headache, nausea or vomiting, blurred vision, and seeing halos around lights. The eye may also appear red and swollen. It’s important to note that these symptoms require immediate medical attention. If left untreated for even a short time, acute closed angle glaucoma can lead to permanent vision loss.
In my experience with patients who have faced this condition, many express confusion about whether their symptoms are related to other issues like migraines or sinus problems. This overlap often leads to delays in seeking treatment. Recognizing these symptoms early can be crucial for preserving vision.
Risk Factors
Several risk factors increase the likelihood of developing acute closed angle glaucoma. Age is a significant factor; individuals over 60 are at higher risk due to age-related changes in eye structure. Family history also plays a critical role; if someone in your family has had glaucoma, your chances increase.
Other risk factors include ethnicity—those of Asian descent are more prone to this type—and hyperopia (farsightedness). Women tend to be at greater risk than men due to anatomical differences in eye structure. Additionally, certain medical conditions such as diabetes or high blood pressure may contribute to an increased risk.
Diagnosis: How Is It Done?
Diagnosing acute closed angle glaucoma typically involves a comprehensive eye examination by an ophthalmologist. The examination includes measuring intraocular pressure using tonometry—a process that evaluates how much pressure is inside the eye.
The doctor will also perform gonioscopy to examine the drainage angle directly. This test involves placing a special lens on the surface of your eye after applying numbing drops. The lens allows the doctor to see whether your drainage angle is open or closed.
Visual field tests may also be conducted to assess any loss of peripheral vision—a common sign associated with glaucoma progression. It’s essential for anyone experiencing symptoms or having risk factors for glaucoma to undergo regular eye exams.
Treatment Options Available
Treatment for acute closed angle glaucoma focuses on lowering intraocular pressure swiftly and preventing future attacks. Medications are often the first line of defense; these may include topical medications like beta-blockers and carbonic anhydrase inhibitors that reduce fluid production within the eye.
In some cases, oral medications such as acetazolamide may be prescribed for immediate relief. Additionally, pilocarpine drops can help open up the drainage angles by constricting the pupil.
However, medication alone may not suffice for long-term management. Laser therapy is frequently recommended as an effective treatment option. Argon laser peripheral iridotomy (ALPI) creates a small hole in the peripheral iris allowing fluid to flow more freely within the eye’s anterior chamber—thereby relieving pressure.
For those with chronic conditions or frequent attacks, surgical intervention might be necessary. Procedures like trabeculectomy create new drainage pathways for fluid release from inside the eye.
Table: Comparison of Treatment Options
| Treatment Type | Description | Effectiveness |
|---|---|---|
| Medications | Topical drops or oral medications that lower IOP. | Effective for immediate relief but not long-term. |
| Laser Therapy | Creates openings in iris for better fluid drainage. | Highly effective; often prevents future attacks. |
| Surgery | Surgical procedures create new drainage pathways. | Effective for chronic cases; requires careful monitoring. |
Preventive Measures
While not all cases of acute closed angle glaucoma can be prevented—especially those tied directly to genetics—certain measures can significantly reduce risks. Regular comprehensive eye exams are vital as they allow early detection and monitoring of intraocular pressure levels.
For those identified at higher risk due to narrow angles or family history, preventive laser procedures might be recommended even before symptoms arise. These proactive steps help mitigate potential future episodes effectively.
Lifestyle changes also play a role; maintaining overall health through regular exercise and a balanced diet supports good ocular health as well as general well-being.
Living with Acute Closed Angle Glaucoma
Receiving a diagnosis of acute closed angle glaucoma can feel overwhelming but understanding how to manage it makes all the difference. Staying informed about one’s condition empowers individuals to take control over their health decisions actively.
Regular follow-ups with an ophthalmologist are crucial for monitoring any changes in vision or intraocular pressure levels post-treatment. Embracing supportive resources—such as local support groups or educational workshops—can provide additional encouragement and information on living well with this condition.
Many patients find it helpful to maintain records of their symptoms and treatments during consultations with healthcare providers; this practice aids in tracking progress over time while ensuring all concerns are addressed promptly.
The Importance of Awareness
Raising awareness about acute closed angle glaucoma is essential not just for those diagnosed but also for society at large. Increased understanding leads to earlier detection and treatment options being sought out by individuals who might otherwise overlook their symptoms until it’s too late.
Education campaigns targeting high-risk populations could significantly impact outcomes by encouraging routine screenings among older adults or those with family histories linked directly back into this dangerous form of glaucoma.
In my experience working alongside healthcare professionals dedicated towards improving public knowledge surrounding ocular diseases—initiatives aimed at enhancing awareness remain paramount towards reducing incidences tied back into preventable blindness caused by conditions like acute closed-angle glaucoma!
Key Takeaways: Acute Closed Angle Glaucoma
➤ Serious Condition: Acute closed angle glaucoma can lead to rapid vision loss.
➤ Recognize Symptoms: Severe eye pain and blurred vision require immediate care.
➤ Risk Factors: Age, family history, and ethnicity increase likelihood of onset.
➤ Treatment Options: Medications, laser therapy, and surgery can manage the condition.
➤ Prevention Matters: Regular eye exams help in early detection and risk reduction.
➤ Prevention Matters: Regular eye exams help in early detection and risk reduction.
Frequently Asked Questions: Acute Closed Angle Glaucoma
What is Acute Closed Angle Glaucoma and how does it develop?
Acute closed angle glaucoma is a medical emergency characterized by a sudden rise in intraocular pressure due to blockage of the eye’s drainage angle. This condition can develop rapidly, often without warning, leading to severe symptoms such as eye pain and blurred vision. The anatomical structure of the eye plays a significant role; individuals with naturally narrow angles are more prone to this condition. Understanding its development is crucial for early detection and intervention.
What are the long-term effects of untreated Acute Closed Angle Glaucoma?
If acute closed angle glaucoma remains untreated, it can lead to irreversible vision loss. The elevated intraocular pressure damages the optic nerve over time, resulting in permanent blindness if not addressed promptly. Additionally, chronic episodes can cause ongoing discomfort and complications in daily activities. Long-term management strategies are essential to mitigate these risks and preserve visual acuity.
How is Acute Closed Angle Glaucoma diagnosed?
The diagnosis of acute closed angle glaucoma typically involves a comprehensive eye examination by an ophthalmologist. This includes measuring intraocular pressure using tonometry, which assesses how much pressure is inside the eye. Gonioscopy is also performed to directly visualize the drainage angle. These diagnostic tools help determine whether the angle is open or closed, guiding treatment decisions effectively.
What lifestyle changes can help manage Acute Closed Angle Glaucoma?
acute closed angle glaucoma. Regular exercise promotes overall eye health and helps maintain healthy blood pressure levels. A balanced diet rich in antioxidants supports ocular health as well. Furthermore, avoiding medications that may dilate pupils and lead to angle closure is crucial for those at risk. Regular follow-ups with an ophthalmologist ensure ongoing monitoring and timely intervention.
Are there any preventive measures for Acute Closed Angle Glaucoma?
acute closed angle glaucoma can be prevented, certain measures may reduce risks significantly. Regular comprehensive eye exams are vital for early detection of high intraocular pressure or anatomical predispositions. For high-risk individuals, preventive laser procedures might be advised even before symptoms appear. Staying informed about one’s risk factors and maintaining regular check-ups contribute greatly to prevention efforts.
Conclusion – What is Acute Closed Angle Glaucoma?
Acute closed angle glaucoma stands out as one of those urgent medical conditions requiring swift action upon symptom onset due primarily because its effects can quickly escalate into irreversible damage without proper intervention! Understanding its causes helps demystify what happens within our eyes while recognizing symptoms encourages timely responses when faced with potential crises ahead!
By being proactive about regular check-ups alongside lifestyle adjustments tailored towards supporting overall health—we stand better equipped against managing risks associated with both current diagnoses & future occurrences alike!